 With hospitals, clinics, and medical offices overwhelmed with treating patients infected with COVID-19, we offer some advice for identifying and caring for those individuals who have difficulty hearing and understanding speech. Hearing loss is a highly prevalent condition especially in elderly populations where according to WHO estimates nearly one third of people aged 65 and older suffer from hearing loss. The most common form of hearing loss, sensorineural hearing loss (caused by damage to the inner ear or nerve from the ear to the brain), strongly impacts a persons ability to follow and participate in a conversation. Hearing loss is not only a matter of not hearing but also a matter of not understanding. Due to the complex nature of sensorineural hearing loss, especially in communication conditions full of ambient sounds, hearing impaired people suffer greatly from not understanding despite knowing that something has been said.
With hospitals, clinics, and medical offices overwhelmed with treating patients infected with COVID-19, we offer some advice for identifying and caring for those individuals who have difficulty hearing and understanding speech. Hearing loss is a highly prevalent condition especially in elderly populations where according to WHO estimates nearly one third of people aged 65 and older suffer from hearing loss. The most common form of hearing loss, sensorineural hearing loss (caused by damage to the inner ear or nerve from the ear to the brain), strongly impacts a persons ability to follow and participate in a conversation. Hearing loss is not only a matter of not hearing but also a matter of not understanding. Due to the complex nature of sensorineural hearing loss, especially in communication conditions full of ambient sounds, hearing impaired people suffer greatly from not understanding despite knowing that something has been said.
In recent years a lot of research has been published showing how hearing loss limits the communication between hearing impaired people and their communication partners. Research has mainly focused on families and friends as communication partners and to a lesser extent addressed other types of communication such as with care providers. 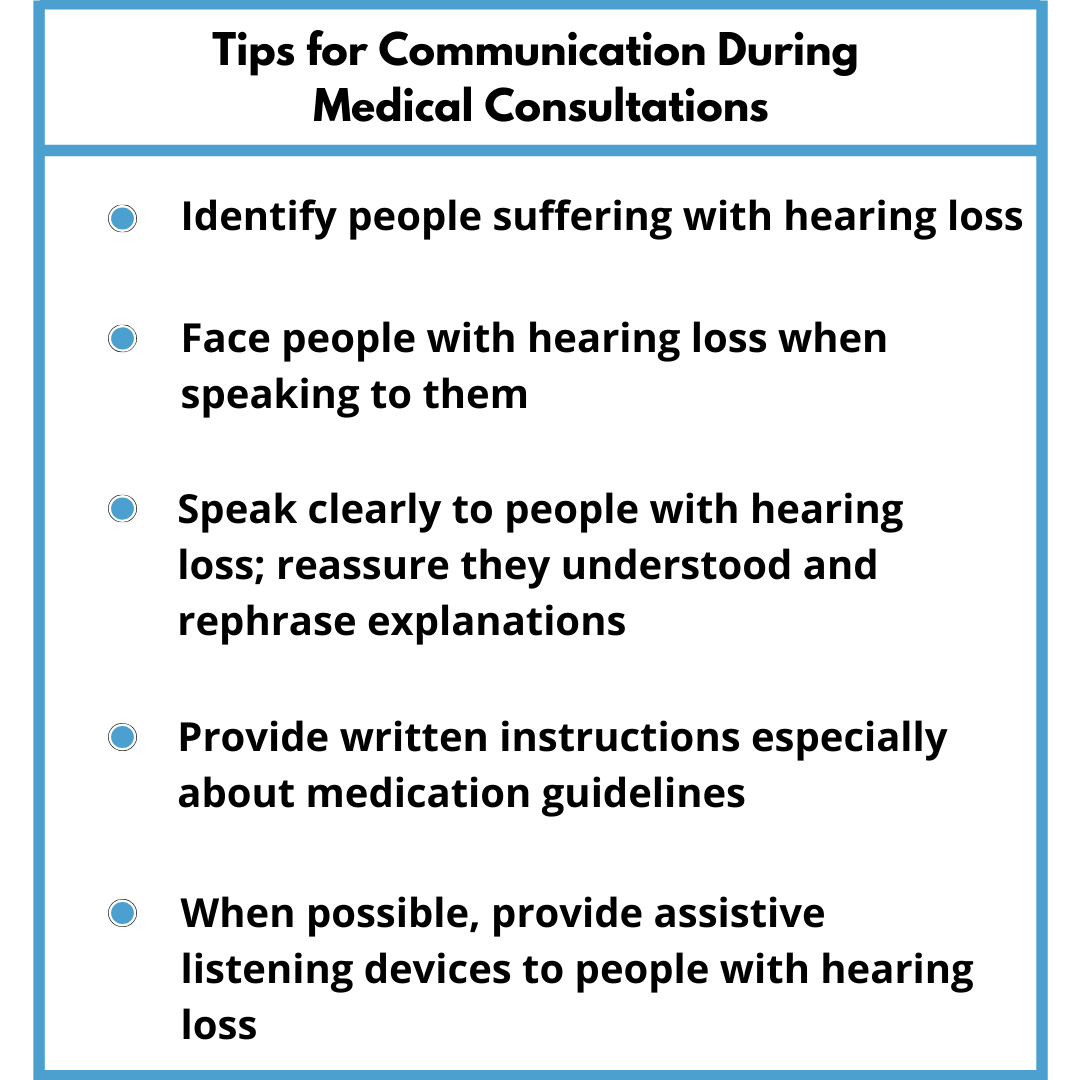 From a social integration perspective, communication with family and friends is most important but other communication situations are very critical and also need to be addressed.
From a social integration perspective, communication with family and friends is most important but other communication situations are very critical and also need to be addressed.
One significant communication situation is in health care settings where good communication has been associated with better outcomes in health care (Blustein, Weinstein, Chodosh, BMJ 2018; Weinstein, 2020 Hearing Journal). Health care consultations often impose significant challenges on the hearing impaired subjects because i) health care settings can be rather noisy with a lot of ambient sounds and multiple talkers especially in hospitals, ii) use of often unfamiliar terminology and context information, iii) often take place without direct facial sight, ie no lip reading to support understanding, iv) take place without any form of amplification supporting audibility to hearing impaired people.
Several recent publications discussed the impact of hearing loss on medical consultations in health care settings. The authors concluded that hearing impaired people are at a much higher risk of misunderstandings and even communication breakdowns in medical consultations. The studies mostly relied on qualitative research using questionnaires and surveys to investigate challenges people with hearing loss are facing in medical consultations. Studies investigated communication challenges in a very large general population using few items questionnaires (Mick, Foley, Lin, 2014, JAGS) in an elderly population using semi-structured interviews (Cudmore, Henn, O’Tuathaigh, Smith, 2017 JAMA) and in a student population using questionnaires (Henn, O’Tuathaigh, Keegan, Smith 2017, J Patient Safety). The studies found significant impact of hearing loss on medical consultations with 30 … (60%) of the participants reporting challenges with mishearing or misunderstanding illness or treatment related information and details on diagnosis and guidelines for medication. Such miscommunications or even communication breakdowns can have significant impact on the outcomes of medical care leading to higher hospital readmissions rates of hearing impaired people compared to normal hearing peers (Chang, Weinstein, Chodosh, Blustein, 2018, JAGS). Shukla et al (Shukla, Nieman, …, Reed 2019, Am J Medical Quality) recently reviewed and summarized the impact of hearing loss on patient-provider communication in hospitalized settings. They identified challenges for all stakeholders involved – from a patient perspective with mishearing medical information and instructions as well as from a care provider perspective with taking medical history from and providing instructions to a patient.
Blustein et al (Blustein, Weinstein, Chodosh, BMJ 2018, see also Shukla et al 2019) discuss the importance of changing communication behavior in medical consultation settings encouraging health care professionals to use the tips in Table 1.
Despite hearing loss having such a strong impact on a person’s ability to follow and participate in a conversation as well as good communication being considered a relevant contributor to good outcomes in health care, hearing loss has rarely been considered in this discussion (Cohen, Blustein, Weinstein, et al 2017, JAGS). Especially in a crisis the world is facing currently with the Coronavirus pandemic, we have to take action and inform health care providers about the importance of addressing hearing loss in medical consultation settings.
Table 1. Tips from the article Tackling hearing loss to improve the care of older Adults by Blustein, Weinstein and Chodosh (2018); BMJ 2018;360:k21 doi: 10.1136/bmj.k21